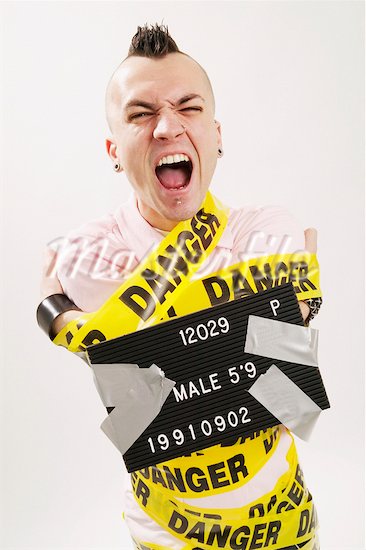
 Teenagers are often characterized as over-emotional, prone to outbursts that confuse their parents and leave teachers reeling.
Teenagers are often characterized as over-emotional, prone to outbursts that confuse their parents and leave teachers reeling.
But a study published in the July issue of the journal Archives of General Psychiatry says 1 in 12 adolescents may in fact be suffering from a real and severe anger problem known as intermittent explosive disorder (IED).
Study author Katie McLaughlin, a clinical psychologist and psychiatric epidemiologist, says IED is one of the most widespread mental health disorders – and one of the least studied.
“There’s a contrast between how common the disorder is and how much we know about it,” she said.
IED is characterized by recurrent episodes of aggression that involve violence, a threat of violence and/or destruction of property, according to the Diagnostic and Statistical Manual of Mental Disorders. It often begins around the age of 12, but scientists don’t know whether it continues into adulthood. (A similar study which focused on adults found 7.2% met the criteria for IED).
“Intermittent explosive disorder is as real or unreal as many psychiatric disorders,” wrote CNN’s mental health expert Dr. Charles Raison in an e-mail. “There are people who get really pissed off really quick and then regret it, just as there are people who get unreasonably sad and depressed. In both cases, but especially with [IED], it’s really just a description of how people behave.”
In this large study, researchers authors interviewed 6,483 adolescents and surveyed their parents. They excluded anyone who had another mental health disorder, such as attention deficit hyperactivity disorder, oppositional defiant disorder (ODD) or conduct disorder (CD).
Of the teenage participants, 7.8% reported at least three IED anger attacks during their life. More than 5% had at least three attacks in the same year.
McLaughlin said one of the most interesting things her team found was that very few of the adolescents who met the criteria for IED had received treatment for anger or aggressive behavior. More research needs to be done to determine if treatments that have been developed for ODD or CD anger issues would apply to IED as well.
Additional research should also look into the risk factors for IED, she said. “We know not that much about course of the disorder… Which kids grow out of it and which kids don’t?”
Source: http://thechart.blogs.cnn.com/2012/07/02/does-your-teen-have-a-severe-anger-disorder/


