By Adam Cook @ Addictionhub.org
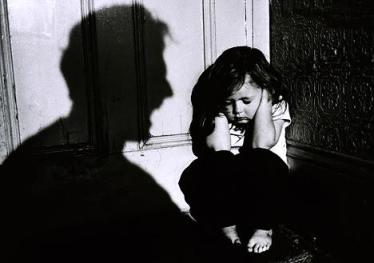
 Domestic violence is more prevalent than you may realize. 95% of the cases involve female victims of male partners, but the female often isn’t the only victim. An estimated 3.2 million children living in America witness incidents of domestic violence annually. Witnessing has an array of meanings. It includes seeing the actual event of physical or sexual abuse occur, hearing threats or other violent noises from another room, observing the aftermath from the abuse like blood, bruises, tears, or broken items, and being aware of the tension in the household like the fear when the abuser is present. The child is like an extension of their abused parent− when the mother gets abused, it’s like the child gets abused. Here are some of the long-term effects of domestic violence on children.
Domestic violence is more prevalent than you may realize. 95% of the cases involve female victims of male partners, but the female often isn’t the only victim. An estimated 3.2 million children living in America witness incidents of domestic violence annually. Witnessing has an array of meanings. It includes seeing the actual event of physical or sexual abuse occur, hearing threats or other violent noises from another room, observing the aftermath from the abuse like blood, bruises, tears, or broken items, and being aware of the tension in the household like the fear when the abuser is present. The child is like an extension of their abused parent− when the mother gets abused, it’s like the child gets abused. Here are some of the long-term effects of domestic violence on children.
Physical Health Problems
Unfortunately, children aren’t always just witnessing these attacks− sometimes they are on the receiving end of it as well. Other physical symptoms of growing up in a violent home include stomachaches, headaches, bedwetting, and inability to concentrate. Experts believe that children who grow up in abusive homes think that violence is an effectual way to resolve conflicts and solve problems. This may result in the child replicating the violence and intimidation that they witnessed when they were younger in their teen and adult relationships, and can lead to the cycle of violence with their children.
PTSD
Exposure to domestic violence as a child can lead to Post-traumatic Stress Disorder. Children’s interpersonal violence exposure wasn’t always recognized as a potential antecedent to PTSD, but now it is acknowledged that extraordinarily stressful events can occur as part of children’s habitual experiences. Recent definitions of trauma stressors now include moments within ordinary circumstances that are capable of causing death, injury, or threaten the well-being of a loved one or the child itself. Signs of PTSD include:
- Reliving the event: Memories of the event can resurface at any given moment, evoking the same feelings of fear and horror that occurred during the actual event. Nightmares, flashbacks, and triggers like seeing, hearing, or smelling something that causes the child to relive the traumatic event are forms of these re-experiencing symptoms.
- Avoiding situations that remind the child of the event: The child may try to avoid situations or people that trigger those memories of a past event of domestic violence. They may keep busy or avoid seeking help because it keeps them from having to think or talk about the event.
- Negative changes in beliefs and feelings: The self-image the child possessed may change, as well as the way they view others. There are many aspects to this symptom, including a belief that the world is completely dangerous and no one can be trusted, or a lack of loving or positive feelings in relationships.
- Hyperarousal: The child may be jittery, irritable, angry, or always alert and on the lookout for danger. Trouble sleeping and concentrating may occur, or they may be startled by loud noises or surprises.
–
If you relocate as a result of a domestic violence situation, be aware that even moving to a new place can have emotional effects on children. If they’re removed from a familiar school or friends, they may face depression and other challenges. This should be addressed in any kind of therapy.
Substance Abuse
Often a matter of coping with the domestic violence and the consequences it brings, children who experience violent and traumatic events use drugs and alcohol to numb the pain and block out the memories. Substance abuse is most likely a learned behavior. Regular alcohol abuse is one of the leading risk factors for partner violence, and the risk of violence increases when both partners abuse drugs or alcohol.
Therapy and Treatment Options
There are numerous organizations that offer several avenues for child victims of domestic violence to address their issues and attempt to heal. Group and individual therapy, as well as dyadic treatments with their non-offending parent are essential components of intervention. The National Domestic Violence Hotline for victims is 1-800-799-SAFE (7233). Their website, www.thehotline.org, provides information about local programs or resources available.
Related Online Continuing Education (CE) Courses:
Domestic Violence: Child Abuse and Intimate Partner Violence is a 2-hour online continuing education (CE) course intended to help healthcare professionals maintain a high state of vigilance and to be well prepared with immediate and appropriate responses when abuse is disclosed.
How Children Become Violent is a 6-hour online continuing education (CE) course that was written for professionals working in the mental health, child welfare, juvenile justice/criminal justice, and research fields, as well as students studying these fields. The authors’ goal is to make a case for the fact that juvenile and adult violence begins very early in life, and it is both preventable and treatable.
Improving Cultural Competence in Substance Abuse Treatment is a 4-hour online continuing education (CE) course that proposes strategies to engage clients of diverse racial and ethnic groups in treatment.
PTSD Vicarious Traumatization: Towards Recognition & Resilience-Building is a 2-hour online continuing education (CE) course that outlines some of the basic differences between primary traumatization, secondary traumatization, VT, and compassion fatigue; discusses many of the signs and symptoms of VT; provides questions for self-assessment of VT; and provides coping suggestions for providers who are involved in trauma work or those who may have VT reactions.
—
 Professional Development Resources is a nonprofit educational corporation 501(c)(3) organized in 1992. Our purpose is to provide high quality online continuing education (CE) courses on topics relevant to members of the healthcare professions we serve. We strive to keep our carbon footprint small by being completely paperless, allowing telecommuting, recycling, using energy-efficient lights and powering off electronics when not in use. We provide online CE courses to allow our colleagues to earn credits from the comfort of their own home or office so we can all be as green as possible (no paper, no shipping or handling, no travel expenses, etc.). Sustainability isn’t part of our work – it’s a guiding influence for all of our work.
Professional Development Resources is a nonprofit educational corporation 501(c)(3) organized in 1992. Our purpose is to provide high quality online continuing education (CE) courses on topics relevant to members of the healthcare professions we serve. We strive to keep our carbon footprint small by being completely paperless, allowing telecommuting, recycling, using energy-efficient lights and powering off electronics when not in use. We provide online CE courses to allow our colleagues to earn credits from the comfort of their own home or office so we can all be as green as possible (no paper, no shipping or handling, no travel expenses, etc.). Sustainability isn’t part of our work – it’s a guiding influence for all of our work.
Earn CE Wherever YOU Love to Be!
We are approved to offer continuing education by the American Psychological Association (APA); the National Board of Certified Counselors (NBCC); the Association of Social Work Boards (ASWB); the American Occupational Therapy Association (AOTA); the American Speech-Language-Hearing Association (ASHA); the Commission on Dietetic Registration (CDR); the Alabama State Board of Occupational Therapy; the Florida Boards of Social Work, Mental Health Counseling and Marriage and Family Therapy, Psychology & School Psychology, Dietetics & Nutrition, Speech-Language Pathology and Audiology, and Occupational Therapy Practice; the Ohio Counselor, Social Worker & MFT Board and Board of Speech-Language Pathology and Audiology; the South Carolina Board of Professional Counselors & MFTs; the Texas Board of Examiners of Marriage & Family Therapists and State Board of Social Worker Examiners; and are CE Broker compliant (all courses are reported within one week of completion).

 It can be difficult to diagnose a substance abuse problem and a co-occurring mental health disorder such as depression, anxiety, or bipolar disorder. It takes time to tease out what might be a mental disorder and what might be a drug or alcohol problem.
It can be difficult to diagnose a substance abuse problem and a co-occurring mental health disorder such as depression, anxiety, or bipolar disorder. It takes time to tease out what might be a mental disorder and what might be a drug or alcohol problem.